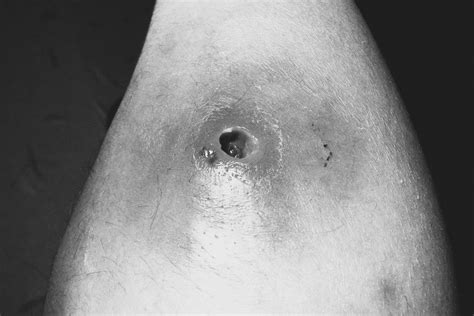
Tunneling wounds are a complex and challenging type of wound that requires specialized care and management. These wounds are characterized by a narrow, sinuous tract or tunnel that extends from the surface of the skin into deeper tissues, often with multiple branches and cavities. Tunneling wounds can be caused by a variety of factors, including trauma, surgery, infection, and underlying medical conditions such as diabetes or vascular disease.
According to the Wound, Ostomy and Continence Nurses Society (WOCN), tunneling wounds are classified as a type of pressure ulcer, which is a localized damage to the skin and/or underlying tissue that usually occur over a bony prominence as a result of pressure, or pressure in combination with shear and/or friction. The prevalence of tunneling wounds is estimated to be around 10-15% of all pressure ulcers, with a higher incidence in patients with limited mobility, such as those with spinal cord injuries or elderly individuals with limited ability to change positions.
Key Points
- Tunneling wounds are characterized by a narrow, sinuous tract or tunnel that extends from the surface of the skin into deeper tissues.
- These wounds can be caused by trauma, surgery, infection, and underlying medical conditions such as diabetes or vascular disease.
- Tunneling wounds are classified as a type of pressure ulcer, with a prevalence of around 10-15% of all pressure ulcers.
- Patients with limited mobility, such as those with spinal cord injuries or elderly individuals, are at higher risk of developing tunneling wounds.
- Early detection and treatment of tunneling wounds are critical to prevent complications and promote healing.
Causes and Risk Factors
Tunneling wounds can be caused by a variety of factors, including mechanical stress, infection, and underlying medical conditions. Mechanical stress, such as pressure, shear, and friction, can cause damage to the skin and underlying tissues, leading to the formation of a tunneling wound. Infection can also play a role in the development of tunneling wounds, particularly in patients with compromised immune systems or those who have undergone surgery. Underlying medical conditions, such as diabetes, vascular disease, and neurological disorders, can also increase the risk of developing tunneling wounds.
Diagnosis and Assessment
Diagnosing tunneling wounds requires a thorough assessment of the wound, including a visual examination, measurement of the wound size and depth, and evaluation of the surrounding tissue. The wound bed should be inspected for signs of infection, such as redness, swelling, and purulent discharge. The wound edges should be evaluated for signs of epithelialization, such as the presence of a scab or granulation tissue. Imaging studies, such as X-rays or MRI, may be ordered to evaluate the extent of the wound and to rule out any underlying conditions that may be contributing to the wound.
| Wound Characteristic | Description |
|---|---|
| Wound size | Measured in centimeters, with a range of 1-10 cm or more |
| Wound depth | Measured in millimeters, with a range of 1-10 mm or more |
| Wound shape | Varies, but often irregular or sinuous |
| Wound edges | May be rolled, thickened, or irregular |
| Wound bed | May be covered with slough, eschar, or granulation tissue |

Treatment and Management

Treating tunneling wounds requires a comprehensive approach that addresses the underlying causes of the wound, promotes a moist wound environment, and prevents further tissue damage. The primary goals of treatment are to promote wound healing, prevent infection, and improve patient outcomes. This can be achieved through a variety of interventions, including debridement, dressing changes, and the use of advanced wound therapies such as negative pressure wound therapy (NPWT) or hyperbaric oxygen therapy (HBOT).
Debridement and Dressing Changes
Debridement, the removal of dead or damaged tissue, is a critical component of tunneling wound care. This can be achieved through surgical debridement, where the dead tissue is removed surgically, or through autolytic debridement, where the body’s natural enzymes break down the dead tissue. Dressing changes are also an essential part of tunneling wound care, as they help to maintain a moist wound environment, promote wound healing, and prevent infection. The type and frequency of dressing changes will depend on the individual patient’s needs and the stage of wound healing.
What is the best way to prevent tunneling wounds?
+Preventing tunneling wounds requires a multifaceted approach that includes regular skin inspections, proper wound care, and management of underlying medical conditions. Patients at high risk of developing tunneling wounds, such as those with limited mobility, should be turned regularly to reduce pressure on the skin and underlying tissues.
How can I promote wound healing in a tunneling wound?
+Promoting wound healing in a tunneling wound requires a comprehensive approach that addresses the underlying causes of the wound, promotes a moist wound environment, and prevents further tissue damage. This can be achieved through a variety of interventions, including debridement, dressing changes, and the use of advanced wound therapies such as NPWT or HBOT.
What are the complications of tunneling wounds?
+Tunneling wounds can lead to a variety of complications, including infection, abscess formation, and osteomyelitis. If left untreated, tunneling wounds can also lead to more serious complications, such as sepsis, amputation, and even death.
In conclusion, tunneling wounds are complex and challenging wounds that require specialized care and management. Early detection and treatment are critical to prevent complications and promote healing. A comprehensive treatment plan that addresses the underlying causes of the wound, promotes a moist wound environment, and prevents further tissue damage is essential for optimal outcomes. By understanding the causes, risk factors, and treatment options for tunneling wounds, healthcare professionals can provide high-quality care and improve patient outcomes.



