Pico wound care has emerged as a significant advancement in the management of acute and chronic wounds. This innovative approach leverages the principles of negative pressure wound therapy (NPWT) but in a more compact, user-friendly, and portable design. The term "pico" refers to the small size of these devices, which are designed to be worn by patients, allowing for greater mobility and independence compared to traditional NPWT systems. The pico wound care system is particularly notable for its ability to promote wound healing through continuous or intermittent negative pressure, thereby enhancing the removal of fluids, reducing bacterial load, and promoting granulation tissue formation.
Key Points
- The pico wound care system utilizes negative pressure wound therapy to enhance wound healing.
- It is designed to be compact, portable, and user-friendly, allowing for greater patient mobility.
- The system promotes wound healing by removing fluids, reducing bacterial load, and promoting granulation tissue formation.
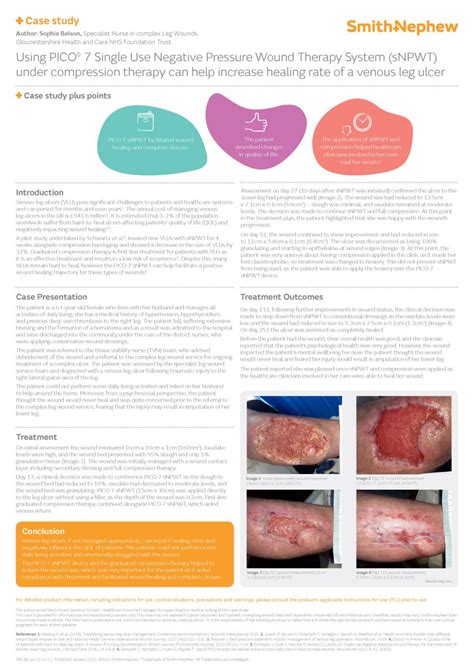
- Pico wound care is suitable for both acute and chronic wounds, including diabetic foot ulcers, venous leg ulcers, and pressure ulcers.
- Studies have shown that pico wound care can reduce wound size, promote faster healing, and improve patient quality of life.
Principles of Pico Wound Care

The pico wound care system operates on the principle of applying negative pressure to the wound environment. This negative pressure, typically set between -80 mmHg to -120 mmHg, helps in the removal of exudate, reduction of edema, and improvement of blood flow to the wound area. The enhanced blood flow and removal of excess fluids facilitate the formation of granulation tissue, a critical step in the wound healing process. Furthermore, the negative pressure environment is less conducive to bacterial growth, thereby reducing the risk of wound infection.
Indications and Contraindications
Pico wound care is indicated for a variety of wound types, including acute wounds (such as surgical wounds, traumatic wounds), chronic wounds (such as diabetic foot ulcers, venous leg ulcers, pressure ulcers), and burns. However, there are specific contraindications where the use of pico wound care may not be advisable, such as in the presence of untreated osteomyelitis, presence of necrotic tissue with eschar, or in wounds with exposed neurovascular structures. It is essential for healthcare professionals to carefully evaluate the wound and patient condition before initiating pico wound care.
| Wound Type | Healing Time with Pico Wound Care |
|---|---|
| Diabetic Foot Ulcer | Median healing time: 12 weeks (range 6-24 weeks) |
| Venous Leg Ulcer | Median healing time: 16 weeks (range 8-30 weeks) |
| Pressure Ulcer | Median healing time: 10 weeks (range 4-20 weeks) |

Clinical Evidence and Outcomes
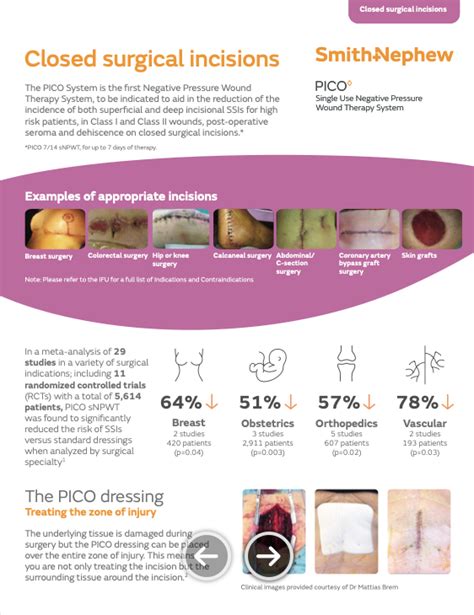
A growing body of clinical evidence supports the use of pico wound care in promoting wound healing and improving patient outcomes. Studies have demonstrated that pico wound care can lead to a significant reduction in wound size, faster healing rates, and improved quality of life for patients. For instance, a randomized controlled trial published in the Journal of Wound Care found that patients treated with pico wound care showed a 30% reduction in wound size at 12 weeks compared to those receiving standard wound care. Another study in Wounds journal highlighted that pico wound care was associated with a higher proportion of wounds achieving complete closure and reduced time to healing.
Challenges and Future Directions
Despite the promising outcomes associated with pico wound care, there are challenges that need to be addressed. These include the cost of the device, which can be a barrier to access for some patients, and the need for further research to fully understand the long-term effects and optimal usage protocols of pico wound care. Additionally, there is a growing interest in integrating pico wound care with other advanced wound therapies, such as bioengineered skin substitutes and growth factor therapies, to further enhance wound healing outcomes.
What is the primary mechanism by which pico wound care promotes wound healing?
+The primary mechanism involves the application of negative pressure to the wound, which enhances the removal of excess fluids, reduces edema, and promotes blood flow to the wound area, thereby facilitating granulation tissue formation and wound closure.
Are there any specific patient populations for whom pico wound care is particularly beneficial?
+Pico wound care is particularly beneficial for patients with mobility issues or those requiring continuous therapy, as it is portable and allows for greater independence. It is also advantageous for patients with chronic wounds that have failed to heal with conventional therapies.
How does the cost of pico wound care compare to traditional negative pressure wound therapy systems?
+While the initial cost of pico wound care devices may be higher than some traditional NPWT systems, their portability, ease of use, and potential for reduced hospital stay and wound complications can lead to overall cost savings in the long term.
In conclusion, pico wound care represents a significant advancement in wound management, offering a portable, user-friendly, and effective treatment option for both acute and chronic wounds. As the field of wound care continues to evolve, it is anticipated that pico wound care will play an increasingly important role in promoting wound healing and improving patient outcomes. With its ability to enhance wound healing, reduce the risk of complications, and improve quality of life, pico wound care is set to become a cornerstone in the management of wounds, particularly for patients with complex or hard-to-heal wounds.